The global health landscape is increasingly dominated by a silent pandemic: noncommunicable diseases (NCDs). Often overshadowed by infectious disease outbreaks, NCDs – including heart disease, stroke, cancer, diabetes, and chronic respiratory diseases – are responsible for a staggering 75% of all deaths worldwide. However, the burden of these diseases is not evenly distributed. Low- and middle-income countries (LMICs) bear the brunt of this epidemic, accounting for over three-quarters of all NCD-related deaths and a shocking 82% of premature deaths from these conditions. This disparity highlights the urgent need for targeted interventions and increased attention to address the unique challenges faced by LMICs in combating NCDs.
The statistics are stark. In 2021 alone, NCDs claimed the lives of 43 million people globally. Of these, 18 million deaths occurred before the age of 70, classified as premature deaths. The overwhelming majority of these premature deaths – nearly 15 million – occurred in LMICs. This loss of life not only has devastating consequences for individuals and families but also undermines economic development and perpetuates cycles of poverty. When individuals in their most productive years are struck down by preventable diseases, it strains healthcare systems, reduces workforce participation, and hinders overall societal progress.
Several factors contribute to the disproportionate burden of NCDs in LMICs. One significant issue is the double burden of disease. These countries often continue to grapple with high rates of infectious diseases while simultaneously experiencing a rapid increase in NCDs driven by factors such as urbanization, globalization, and lifestyle changes. This dual challenge strains already fragile healthcare systems that are often ill-equipped to handle the complex and long-term management of chronic conditions.
Furthermore, access to healthcare services for NCD prevention, early detection, and treatment is often limited in LMICs. This includes a lack of access to affordable medications, diagnostic tools, and specialized medical professionals. As a result, many individuals with NCDs are diagnosed late in the course of their illness, when treatment options are more limited and outcomes are poorer. Palliative care, which is crucial for managing the symptoms and improving the quality of life for individuals with advanced NCDs, is also often inadequate or unavailable in these settings.
The five major modifiable risk factors for NCDs – tobacco use, physical inactivity, the harmful use of alcohol, unhealthy diets, and air pollution – are often more prevalent or have a greater impact in LMICs. For example, the aggressive marketing of tobacco and unhealthy foods by multinational corporations often targets these vulnerable populations. Similarly, rapid urbanization can lead to more sedentary lifestyles and increased exposure to air pollution. Addressing these risk factors requires comprehensive public health policies and multisectoral action.
The economic consequences of NCDs in LMICs are substantial. The cost of treating these chronic conditions can be catastrophic for individuals and families, often leading to financial hardship and pushing households further into poverty. At a national level, the economic burden of NCDs includes lost productivity, increased healthcare expenditures, and reduced economic growth. Investing in NCD prevention and control is not only a health imperative but also a sound economic strategy.
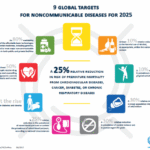
The World Health Organization (WHO) has called for urgent government action to meet global targets for reducing the burden of NCDs. This includes implementing evidence-based interventions such as taxation on tobacco and sugary drinks, promoting healthy diets and physical activity, improving access to essential medicines and technologies, and strengthening healthcare systems to provide integrated NCD care. International cooperation and development assistance are also crucial in supporting LMICs to address this growing epidemic.
Addressing the disproportionate burden of NCDs in LMICs requires a concerted effort from governments, international organizations, civil society, and the private sector. By prioritizing prevention, strengthening healthcare systems, addressing risk factors, and ensuring equitable access to care, it is possible to mitigate the devastating impact of these silent killers and promote healthier and more prosperous societies.