By The Scroll Reporter
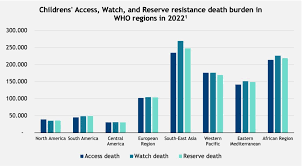
ABOUT one million children in Africa died of antimicrobial resistance (AMR)-associated complications in 2022, with many of these deaths being linked to the use of Watch antibiotics (drugs with a high risk of resistance) and Reserve antibiotics (last-resort treatments for severe, multidrug-resistant infections).
Globally, over three million children lost their lives in 2022 due to AMR-related infections – more than 752,000 children in Southeast Asia and 659,000 children in Africa, with over a million and a half more in other regions of the world died of AMR-associated complications, according to a report presented at the Congress of the European Society of Clinical Microbiology and Infectious Diseases (ESCMID Global 2025) held in Vienna, Austria recently.
The study underscores the urgent need for both regional and global strategies to combat paediatric AMR, particularly in high-burden areas such as South-East Asia and Africa. AMR poses a critical threat to children, who are highly vulnerable to infections.
“While the rise in use of Watch and Reserve antibiotics may be necessary in response to the concurrent rise in drug-resistant infections, the sharp rise in use of these drugs presents several serious long-term risks”, commented Professor Joseph Harwell, study co-author and Senior Clinical Director at Clinton Health Access Initiative (CHAI).
“Their increased use, especially without careful oversight, elevates the risk of resistance and limits future treatment options. If bacteria develop resistance to these antibiotics, there will be few, if any, alternatives for treating multidrug-resistance infections.”
AMR represents a global challenge
- 4.95 million people who died in 2019 suffered from drug-resistant infections.
- AMR directly caused 1.27 million of those deaths.
- 1 in 5 of those deaths occurred among children under 5 years old.
According to the Institute for Health Metrics and Evaluation (IHME), In Zimbabwe in 2019, there were 3,900 deaths attributable to AMR and 15,800 deaths associated with AMR.
- Zimbabwe was among the highest 10 countries in age-standardized mortality rate per 100,000 population associated with AMR across 204 countries.
- The number of AMR deaths in Zimbabwe is higher than deaths from neoplasms, maternal and neonatal disorders, diabetes and kidney diseases, enteric infections, and unintentional injuries.
Children are consistently neglected in global health despite their disproportionate suffering and vulnerability, a cause that CHAI has been a key advocate for being a founding member and a strategic partner with WHO for the Global Accelerator for Paediatric formulations (GAP-f), which focuses on improving access to paediatric medicines.
Addressing this issue requires urgent and coordinated action at both regional and global levels. Even though countries like Cote d’Ivoire, Ghana, Kenya, Malawi, South Africa and Tanzania have made strides to improve surveillance systems and national policies, more must be done to improve health outcomes for children.
Several factors contribute to the severity of AMR in low- and middle-income countries, including overcrowded hospitals, poor sanitation, and weak infection prevention measures that facilitate the spread of resistant pathogens within healthcare settings and communities.
Due to a lack of diagnostic tools and concerns over misdiagnosis, overuse and misuse of antibiotics are also widespread in these regions.
Additionally, many low- and middle-income countries lack effective national surveillance and antimicrobial stewardship programs, making it difficult to track resistance trends and establish effective treatment protocols.
Between 2019 and 2021, the use of Watch antibiotics increased by 160 percent in Southeast Asia and 126 percent in Africa. During the same period, the use of Reserve antibiotics rose by 45 percent in Southeast Asia and 125 percent in Africa.
“Global and national surveillance on AMR must adopt a ‘One Health’ approach, linking human health programs to animal and environmental factors, with cost-effective systems that can inform treatment guidelines and measure the impact of control interventions” said Professor Harwell.
“On a regional level, we urge policymakers to mandate hospital-based antimicrobial stewardship programs in all paediatric healthcare facilities. Improved age classifications will also enhance our understanding of important differences in resistance rates across the age categories, as well as pediatric-specific resistance mechanisms.
“Additionally, we urge the implementation of national guidelines to ensure routine surveillance informs antibiotic use.”
Source: Cliton Health Access Initiative with additional reporting from The Scroll